Macular edema Treatment is a serious eye condition that can really affect your vision and life. But, there are new treatments that can help. Let’s look at the latest ways to treat macular edema and how they can improve your sight.
Do you know what can cause macular edema? Knowing the causes is key to managing and preventing it. We’ll explore the medical conditions, lifestyle choices, and genetics that might lead to macular edema.
Understanding Macular Edema: Causes and Risk Factors
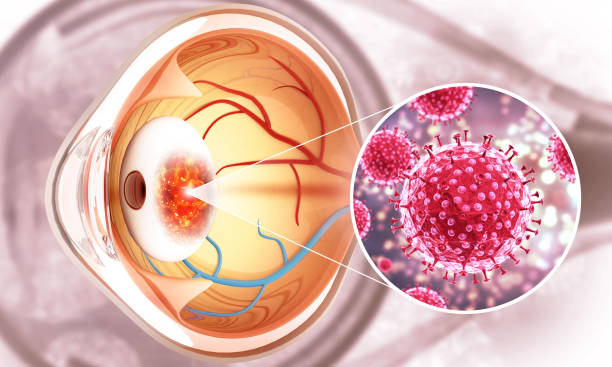
Macular edema is a serious eye condition. It happens when the macula, the retina’s center, swells or thickens. This can cause blurry or distorted vision, making simple tasks hard.
Knowing what causes macular edema is key. It helps prevent and manage the condition.
Common Medical Conditions Leading to Macular Edema
- Diabetic retinopathy: Uncontrolled diabetes can harm the retina’s blood vessels. Fluid leaks into the macula.
- Age-related macular degeneration (AMD): This age-related condition can cause macular edema, especially in its advanced stages.
- Retinal vein occlusion: Blockages in the retinal veins lead to fluid buildup in the macula.
- Uveitis: Eye inflammation, often from another condition, can trigger macular edema.
Lifestyle Factors That Increase Risk
Medical conditions aren’t the only risk. Lifestyle choices can also play a part. These include:
- Smoking: Tobacco use raises the risk of macular edema, especially in those with eye conditions.
- Obesity: Being overweight can affect fluid balance, leading to macular edema.
- Lack of exercise: Not being active can harm blood circulation and increase macular edema risk.
Genetic Predisposition and Age-Related Factors
Some people may be more likely to get macular edema due to genetics. As we age, our eyes change, raising the risk. Regular eye exams are crucial.
Signs and Symptoms of Macular Edema
Macular edema is a condition where fluid builds up in the macula. This part of the retina is key for sharp vision. Knowing the signs is important for early treatment.
One common sign is blurred central vision. It makes tasks like reading and driving hard. You might also see distorted or wavy central vision, where lines seem bent.
Another symptom is changes in color perception. People with macular edema might see less color or have trouble telling colors apart. This can really affect daily life.
Macular edema can also cause blind spots or dark areas in your vision. These spots can make it hard to read or move around safely.
The severity of these symptoms can vary. Early treatment is key to managing the condition. It helps keep your vision and daily life on track.
Retinal Swelling Treatment at Home
While you need a doctor for macular edema, there are home steps to help. These include:
- Eating a diet full of eye-friendly nutrients like lutein and omega-3 fatty acids
- Wearing sunglasses or using computer glasses to block blue light and UV
- Doing eye exercises and taking breaks from screens
- Managing health issues like diabetes that can lead to macular edema
Home remedies can help, but seeing an eye doctor is essential. They can give you a treatment plan to stop vision loss and improve your eyes.
| Symptom | Description |
|---|---|
| Blurred Central Vision | Difficulty in tasks requiring fine visual acuity, such as reading, driving, or recognizing faces. |
| Distorted or Wavy Vision | Straight lines may appear bent or curved due to fluid buildup in the macula. |
| Changes in Color Perception | Reduction in color vibrancy or altered ability to distinguish certain hues. |
| Blind Spots or Dark Areas | Development of blind spots or dark areas within the central vision, making it challenging to perform tasks that require clear, unobstructed sight. |
Diagnostic Procedures and Tests for Macular Edema
Macular edema is a complex eye condition that needs a detailed check-up to find the right treatment. Doctors use advanced imaging and tests to see how bad it is. This helps them decide the best course of action.
Optical Coherence Tomography (OCT)
Optical coherence tomography (OCT) is a key tool for diagnosing macular edema. It’s a non-invasive method that uses light to create detailed images of the retina. OCT scans can show how thick the macula is, helping doctors spot swelling or fluid buildup.
Fluorescein Angiography
Fluorescein angiography is another crucial test for macular edema. It involves injecting a fluorescent dye into the blood and then taking pictures as it moves through the eye’s blood vessels. These pictures can show if there’s any leakage or abnormal blood flow that might be causing the edema.
Visual Acuity Tests
Eye doctors also use visual acuity tests to see how macular edema affects vision. These tests check how sharp and clear a person’s eyesight is, often using an eye chart. By tracking changes in vision, doctors can see how well treatments are working.
By using these tests together, doctors can fully understand a patient’s macular edema. This helps them create a treatment plan that works best for each person. It’s all about keeping vision sharp and improving eye health.
Modern Macular Edema Treatment Options
People with macular edema, a swelling in the retina’s center, now have many treatment options. These new therapies aim to fix the root causes of the problem. They offer hope for better vision and eye health.
Intravitreal injections are a main treatment for macular edema. These injections go straight into the eye. They carry medicines that cut down inflammation and fluid buildup. Anti-VEGF drugs are often used because they work well for many patients.
Laser therapy is also a big help. It uses light to seal off leaking blood vessels. This can ease symptoms and stop vision loss.
Some people might need oral medicines. These treatments tackle the main health issues that lead to macular edema, like diabetes or high blood pressure.
Finding the right treatment for macular edema depends on the patient’s needs and the cause of their condition. Doctors work with patients to create a plan. They use the newest macular edema treatment injection and other cutting-edge methods.

“The key to successful macular edema treatment is early intervention and a personalized approach that addresses the underlying cause of the condition.”
Anti-VEGF Therapy: The Gold Standard Treatment
For many, anti-VEGF therapy is the top choice for treating macular edema. These medicines target and block VEGF proteins. This stops the abnormal blood vessel growth and fluid leakage that cause macular edema.
Types of Anti-VEGF Medications
The main anti-VEGF drugs used are Aflibercept, Bevacizumab, and Ranibizumab. These are given as intravitreal injections right into the eye. This method ensures the medication reaches the affected area effectively.
Treatment Schedule and Duration
- Patients usually get injections every month or every other month. The exact schedule and number of treatments vary based on the case and response.
- The treatment plan is adjusted as needed. This is based on ongoing checks and assessments to ensure the best results.
Expected Outcomes and Success Rates
Studies show anti-VEGF therapy works well in improving vision and reducing macular edema. About 70-80% of patients see a big improvement in their vision and less fluid in the macula. This makes it the main treatment for macular edema.
| Anti-VEGF Medication | Typical Dosage | Success Rate in Improving Vision |
|---|---|---|
| Aflibercept | 2 mg every 4-8 weeks | 75-80% |
| Bevacizumab | 1.25 mg every 4 weeks | 70-75% |
| Ranibizumab | 0.3 mg every 4 weeks | 75-80% |
Ophthalmologists use anti-VEGF therapy to manage macular edema. This helps patients keep and improve their vision. It greatly improves their quality of life.
Corticosteroid Treatments and Their Applications
Corticosteroid treatments are a valuable option for managing macular edema. These anti-inflammatory medications can be given as intravitreal implants or eye drops. They offer targeted relief for those with this condition.
Intravitreal corticosteroid implants, like Ozurdex and Iluvien, slowly release the drug over time. They provide sustained treatment for macular edema. Clinical trials show they improve visual acuity and reduce retinal thickness.
Topical corticosteroid eye drops, such as loteprednol etabonate and difluprednate, are also used. These drops are more convenient and less invasive than implants. However, their effects may not last as long.
Corticosteroid treatments work by reducing inflammation, a main cause of macular edema. By targeting inflammation, these therapies can reduce swelling and fluid buildup in the macula. This can improve vision for patients.
But, corticosteroid treatments have potential side effects. These include increased eye pressure, cataract formation, and infection risk. Healthcare professionals must monitor and manage these risks. The choice to use corticosteroids depends on the patient’s specific needs and risks.
In summary, corticosteroid treatments, whether implants or eye drops, are key in managing macular edema. Understanding their uses and potential side effects helps healthcare providers and patients make the best treatment plan.

Laser Photocoagulation: When and Why It’s Used
Laser photocoagulation is a treatment for macular edema, a condition where fluid builds up in the retina. This laser therapy can effectively treat swelling and prevent vision loss.
Different Types of Laser Treatments
Ophthalmologists use several laser techniques for macular edema treatment:
- Focal laser photocoagulation – This method uses a precise laser beam to seal off leaking blood vessels and reduce fluid in the macula.
- Grid laser photocoagulation – The laser is applied in a grid pattern to affected retina areas, controlling fluid buildup.
- Subthreshold micropulse laser – This advanced technique uses brief, low-intensity laser pulses to stimulate the retina without visible damage.
Recovery and Follow-up Care
Laser photocoagulation is usually done as an outpatient procedure. Patients feel little discomfort. After treatment, vision changes may occur but usually go away in a few days.
Patients need regular check-ups with their ophthalmologist. This is to see how well the laser therapy is working and to address any complications or the need for more treatments.
Laser photocoagulation is a key treatment for macular edema and retinal swelling. It works best when combined with other treatments like anti-VEGF injections or corticosteroids. By choosing the right laser technique and tailoring treatment plans, ophthalmologists can help patients keep or even improve their vision.
Surgical Interventions for Severe Cases
When macular edema gets severe or doesn’t go away, surgery might be needed. Vitrectomy surgery is one option. It removes the vitreous gel to fix the problem. This surgery is small and can help save your vision.
Vitrectomy is suggested when other treatments fail. This includes:
- Macular edema that doesn’t get better with anti-VEGF or corticosteroids
- Tractional macular edema from the retina being pulled
- Macular edema with vitreous hemorrhage or traction
The surgery removes the vitreous gel and fixes other issues like epiretinal membranes. It’s done under local anesthesia. It’s safe and often improves vision and reduces edema.
| Surgical Procedure | Potential Benefits | Potential Risks |
|---|---|---|
| Vitrectomy Surgery | Improved visual acuityReduced macular edemaAlleviation of underlying conditions | InfectionRetinal detachmentCataract formation |
Surgery is for severe cases of macular edema. It’s a good option for those who haven’t seen improvement. Always talk to an eye doctor about the risks and benefits.

Managing Diabetic Macular Edema
Diabetic macular edema is a serious issue linked to diabetic retinopathy. Keeping blood sugar levels in check is vital. This helps prevent more damage to the macula, which is key for clear vision.
Blood Sugar Control
Following a strict diabetes management plan is crucial. This includes checking blood sugar often and eating right. Working with your healthcare team to adjust your plan is important.
Combination Therapy Approaches
Often, a mix of treatments works best for diabetic macular edema. This might include anti-VEGF medications, corticosteroid treatments, and laser photocoagulation. The right treatment depends on how severe it is and how you’ve responded to other treatments.
By taking a comprehensive approach, you can protect your vision. Regular check-ups and teamwork with your healthcare team are key to success.
“The key to managing diabetic macular edema is a comprehensive approach that addresses both the underlying causes and the specific manifestations of the condition.”
Prevention Strategies and Lifestyle Modifications
Macular edema can be tough to deal with, but there are ways to lower your risk. Getting regular eye exams is key. They help catch problems early and start treatment quickly, which can make a big difference.
Eating right and staying active are also important. Foods full of antioxidants, like leafy greens and citrus fruits, can help your eyes. Omega-3 fatty acids are good too. Plus, exercise helps manage health issues like diabetes and high blood pressure, which can lead to macular edema.
If you have macular edema, managing your health is crucial. Keeping blood sugar levels in check is especially important for diabetic macular edema. Working with your doctor, you can create a plan that includes medicine and lifestyle changes. This can help you see better.
FAQ
What is macular edema?
Macular edema is when the macula, the part of the retina for sharp vision, swells. This swelling can blur your vision, making it hard to read, drive, or see faces clearly.
What are the common causes of macular edema?
Many things can cause macular edema, like diabetes, age-related macular degeneration, and eye surgery problems. Smoking and being overweight can also raise your risk.
What are the symptoms of macular edema?
Symptoms include blurry vision, wavy vision, trouble with colors, and being too sensitive to light. These symptoms can really affect your daily life.
How is macular edema diagnosed?
Doctors use eye exams and tests like OCT and fluorescein angiography to diagnose it. These help find out what’s causing it and how bad it is.
What are the treatment options for macular edema?
Treatments include injections, laser therapy, and sometimes surgery. The best plan depends on the cause and how severe it is.
How effective are anti-VEGF injections for treating macular edema?
Anti-VEGF injections are very effective for many cases. They stop abnormal blood vessels and reduce swelling. Studies show they can greatly improve vision and prevent further loss.
When is laser photocoagulation used for macular edema?
Laser therapy is used for some types, like diabetic retinopathy. It seals blood vessels and reduces swelling. It’s often used with other treatments for best results.
What are the surgical options for severe macular edema?
For severe cases, surgery like vitrectomy might be needed. It removes the vitreous gel to reduce swelling and help the macula heal.
How can diabetic patients manage their macular edema?
Keeping blood sugar levels in check is key. A treatment plan that includes injections, laser, and possibly corticosteroids can help manage it and protect your vision.
Can macular edema resolve on its own?
Sometimes, mild cases might get better without treatment if the cause is fixed. But, most cases need treatment to prevent vision loss. Seeing an eye doctor is important if you think you have it.
